What is congenital glaucoma?
The optic nerve is a nerve cord composed of more than one million nerve fibres that connect the retina to the brain. In order to ensure good vision, it is essential that the optic nerve is healthy. Glaucoma encompasses a group of ocular diseases that cause progressive damage to the optic nerve. This damage can result in a reduced visual field and even a complete loss of vision if the condition is not treated.
It is common in adulthood, but some forms of glaucoma, such as congenital glaucoma, only occur in childhood. This is a very rare condition affecting 1 out of every 30,000 live births, but it can cause severe and irreversible loss of vision in children who are affected.
What causes congenital glaucoma?
There is a space inside the eye known as the anterior chamber. This space is full of a clear fluid called aqueous humour that bathes the structures of the eye and maintains its optical properties. It constantly enters and exits the anterior chamber. It drains through the angle formed by the cornea and the iris. The function of this angle is to allow the aqueous humour to flow out of the eye and ensure that the intraocular pressure is stable and does not damage the optic nerve. It is therefore essential that the angle remains open so that the aqueous humour can drain from the eye.
In congenital glaucoma, the intraocular pressure increases because there is a birth defect in the development of the angle of the eye as a result of poor development of the eye. This means that the aqueous humour cannot flow out normally, so the intraocular pressure increases and leads to optic nerve damage.
How is it diagnosed?
Congenital glaucoma is detected through a full eye examination, which is usually carried out under sedation in the operating theatre in the case of babies and children under three years of age.
The examination consists of:
- Examination of the front part of the eye: This aims to assess the condition of the cornea and the angle and then determine the most appropriate surgical procedure for each case.
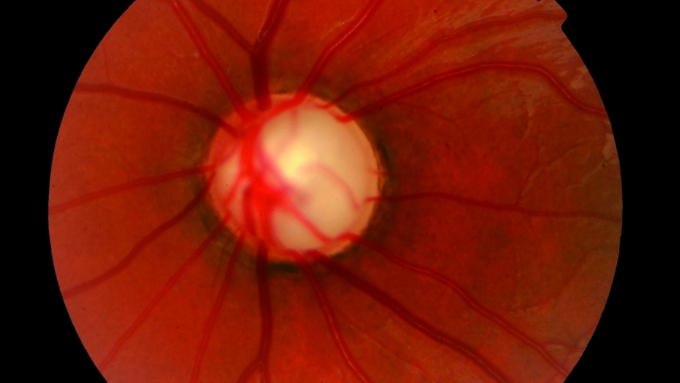
- Examination of the fundus: After dilating the pupils with eye drops, the ophthalmologist looks through a special magnifying lens to examine the retina and optic nerve and identify any signs of damage. Glaucoma causes a progressive loss of nerve fibres from the optic nerve, resulting in a gap (excavation) that increases in size as the disease develops.
- Tonometry: This is performed to measure eye pressure. To perform this test, the ophthalmologist applies some drops to numb the eyes and then places an instrument on the eye to measure the pressure. Normal ocular pressure is between 10 and 20 mm of mercury.
Symptoms
Given that congenital glaucoma normally appears between birth and three years of age, parents are usually the ones to notice that the child is bothered by light (also known as photophobia), has watery eyes (epiphora) and tends to keep his or her eyes closed (blepharospasm). These are the typical symptoms of congenital glaucoma, but as the disease develops, the appearance of the eyes may change due to the increased intraocular pressure; they may appear more opaque and larger than normal, especially if one eye is affected more than the other.
This opacity occurs as a result of the loss of transparency of the cornea, which is the layer at the front of the eye that is damaged by the increased intraocular pressure. The eye also gets bigger due to tissue distension caused by the increased pressure.
Associated treatments
Treating congenital glaucoma in its early stages can slow the development of the disease. However, early diagnosis and treatment are essential.
This type of glaucoma is normally treated with surgery to correct the angle defect that affects the child. If this is carried out early, visual recovery may be good. Treatment usually starts with a range of eye drops and medication to keep the intraocular pressure as stable as possible until surgery is performed.
The type of surgery will depend on the condition of the cornea, as mentioned above; goniotomy is performed if the cornea is transparent and the angle is visible and trabeculectomy is carried out if the cornea is opaque. Both techniques are designed to open the angle defect that affects these children so that it functions properly.
It may have to be performed several times to achieve a reduction in intraocular pressure.
Trabeculectomy involves the extraction of a small amount of tissue to create a new channel for fluid to drain from the eye.
A valve implant is a type of plastic tube that connects the interior of the eye with the exterior, allowing fluid outflow from the eye. Only one eye is operated on at a time. The success rate is 60–80%, but if the opening closes over time, a new operation may be required. Following surgery, the patient must apply eye drops to prevent inflammation and infection.
What is the visual prognosis for children affected by congenital glaucoma?
The visual prognosis for children with congenital glaucoma depends on a number of factors, including:
The time of diagnosis: the prognosis is worse if the condition is diagnosed at birth or if the child has high pressure for many months and is not treated.
Whether or not the cornea is affected: if the patient’s cornea is affected, a corneal transplant may be required in addition to glaucoma surgery.
However, if an early diagnosis is made and treatment is carried out within the first few months of life, good control can be achieved until adulthood.
How should I apply drops to a child with glaucoma?
If your child has been prescribed eye drops to treat glaucoma, you should follow the instructions provided by the ophthalmologist. The proper administration of medication for glaucoma can improve its effectiveness and reduce the risk of side effects. To apply them correctly, follow these steps:
First, wash your hands.
Hold the bottle upside down.
Tilt the child’s head back.
Hold the bottle with one hand and position it as close to the eye as possible, without actually touching the eye.
Using your other hand, pull down the child’s lower eyelid. This will create a small pocket between the eye and the eyelid.
Apply one drop to this small pocket. If the child has been prescribed more than one drop, wait at least five minutes before applying the second drop (repeat the above steps).
Close the child’s eye or lightly press the lower eyelid with your finger for at least one minute. Either of these measures will help ensure that the drops stay in the eye and prevent them from draining out of the tear duct, thus reducing the risk of side effects.
What research is being conducted in the field of glaucoma?
Research is under way to find new techniques and treatments to detect, treat and prevent vision loss in people with glaucoma. For example, studies have discovered genes that can help explain how glaucoma damages the eye. Studies are also being carried out to learn more about who is most likely to develop glaucoma, when to start treatment for people with high ocular pressure and what treatment should be used first.
Specialists who treat this pathology
FAQs
No very complex or painful examinations are required to detect glaucoma and determine its type and stage. The most important tests when making the diagnosis include an examination of the optic nerve –either directly or using automated tests such as the OCT– and the measuring of intraocular pressure (tonometry). In addition to these, a visual field test is performed to determine the stage of the disease, visualisation of the angle formed by the cornea, iris and sclera to classify the type of glaucoma (gonioscope) and measurement of the corneal thickness, as this can have an impact on intraocular pressure (pachymetry).
Glaucoma causes a progressive decrease in the patient’s visual field, and his or her peripheral vision is gradually reduced. It is therefore difficult to notice this gradual loss until the disease is at an advanced stage and the visual field has been greatly and irreversibly reduced.
The myth of people with glaucoma seeing a black tunnel is not true, as the “appearance” of the disease varies depending on each person and the extent to which the visual field is affected. Some patients describe blurred vision, mistiness or blind spots, although they often find it difficult to explain what is wrong and may confuse glaucoma with other eye diseases such as cataracts.
It is an important factor in glaucoma, although the genetic bases of the disorder are heterogeneous: there are some cases of direct transmission from generation to generation (such as congenital glaucoma) and other cases of complex inheritance (e.g. pseudoexfoliation glaucoma) where a higher percentage of sufferers in the same family than the population average is observed. In both circumstances, genetic studies provide the opportunity to detect possible future cases of glaucoma.
While genetic research continues to progress to increase knowledge in this field, it is important for patients with a family history of glaucoma to be aware of the greater risk they are at to suffer the disease. It is therefore recommendable for people with sufferers of glaucoma in their family (parents, siblings and/or children) to take annual ophthalmological controls from the age of 40 at the very latest.
IMO Institute of Ocular Microsurgery
Josep María Lladó, 3
08035 Barcelona
Phone: (+34) 934 000 700
E-mail: international@imo.es
See map on Google Maps
By car
GPS navigator coordinates:
41º 24’ 38” N – 02º 07’ 29” E
Exit 7 of the Ronda de Dalt (mountain side). The clinic has a car park with more than 200 parking spaces.
By bus
Autobus H2: Rotonda de Bellesguard, parada 1540
Autobus 196: Josep Maria Lladó-Bellesguard, parada 3191
Autobuses H2, 123, 196: Ronda de Dalt – Bellesguard, parada 0071
How to arrive at IMO from:
IMO Madrid
C/ Valle de Pinares Llanos, 3
28035 Madrid
Phone: (+34) 910 783 783
See map in Google Maps
Public transport
Metro Lacoma (líne 7)
Autobuses:
- Lines 49 & 64, stop “Senda del Infante”
- Line N21, stop “Metro Lacoma”
Timetables
Patient care:
Monday to Friday, 8 a.m. to 9 p.m.
IMO Andorra
Av. de les Nacions Unides, 17
AD700 Escaldes-Engordany, Andorra
Phone: (+376) 688 55 44
See map in Google Maps
IMO Manresa
C/ Carrasco i Formiguera, 33 (Baixos)
08242 – Manresa
Tel: (+34) 938 749 160
See map in Google Maps
Public transport
FGC. Line R5 & R50 direction Manresa. Station/Stop: Baixador de Manresa
Timetables
Monday to Friday, 09:00 A.M – 07:00 PM